Track Policies in Your State with the Palliative Care Policy GPS

As more states explore opportunities to increase palliative care access to their residents with serious illness, a centralized mechanism to review activity and identify promising approaches can accelerate progress. The Palliative Care Policy GPS (GPS) is a new online and publicly accessible database that tracks state policies on palliative care and related services. The GPS provides health care professionals, policymakers, palliative care champions, payers, and purchasers with a way to search, compare, gain new ideas, and stay up-to-date on policy developments, while also encouraging innovative state policymaking on palliative care issues.
Introduction
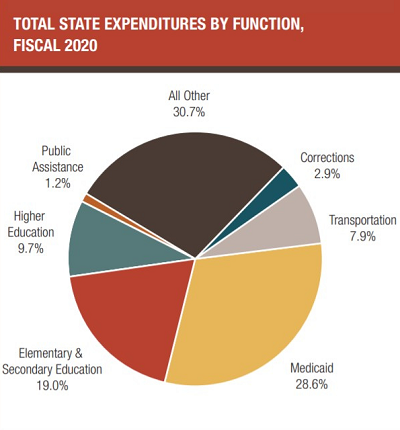
In the last several years, the opportunity that state policy presents in advancing palliative care access and quality has grown increasingly clear. States are deeply committed to improving the quality of care for their most vulnerable residents, and they have many levers to promote palliative care. This includes their key roles in purchasing health care for both Medicaid beneficiaries and their own state employees, as well as their multi-faceted role in regulating health care providers.
States are deeply committed to improving the quality of care for their most vulnerable residents, and they have many levers to promote palliative care.
Meanwhile, states are under enormous pressure as health care expenditures (accounting for approximately 1/3 of state budgets) have continued to grow, with a disproportionate amount of Medicaid spending being directed towards the high-need, high-cost population. And the COVID-19 pandemic has exacerbated the financial pressure on states, as they have not only seen an increase in Medicaid/CHIP enrollment, but also increased obligations around pandemic response, unemployment benefits, etc. – all while grappling with a decreased revenue base.
In looking for innovative solutions to address rising health care costs and improve care for their residents, states have increasingly begun to recognize the value that palliative care can deliver.
In looking for innovative solutions to address rising health care costs and improve care for their residents, states have increasingly begun to recognize the value that palliative care can deliver. State policymakers have introduced hundreds of bills and written regulations that address different components of palliative care over the last decade, such as payment, public awareness, and quality, and the National Academy for State Health Policy (NASHP) is growing its resources to support these efforts. As these policies have proliferated, there has been significant heterogeneity with regards to where and how palliative care is defined, which services or clinical capabilities are promoted, and what populations are supported. Part of this is due to the fact that states are very different from each other with regards to their priorities, structures, and resources for this work; and part of this reflects the emergent nature of palliative care itself, as the field continues to develop and refine its own standards.
Tracking State Policy Developments
Until now, there has not been a single place to house, track, and compare state policy developments regarding palliative care (including in what areas and the success rate of legislative efforts), and its impact on care for people living with serious illness, leaving palliative care champions with little information for decision-making and advocacy.
The new Palliative Care Policy GPS creates a centralized repository to track and analyze these many palliative care policies across the entire United States.
To address this gap, the new “Palliative Care Policy GPS” (GPS) creates a centralized repository to track and analyze these many palliative care policies across the entire United States. The product of a partnership between between CAPC and the Solomon Center for Health Law and Policy at Yale Law School, the goal of the GPS is to support research and encourage policy innovation aimed at ameliorating disparities in access and quality. We have seen the power of similar vehicles, such as the Sabin Center for Climate Change Law’s “Climate Reregulation Tracker” or the National Conference of State Legislatures’ numerous searchable bill tracking databases, in identifying promising policy initiatives and accelerating innovation.
Before we move on, let's define a few key terms:
Laws and Legislatures
Laws are created when state legislatures—or, looking to the federal level, the U.S. Congress—write and pass bills that are then signed by the executive branch (governors at the state level and the president at the federal level).
Regulations
Regulations are created by administrative agencies at the state and federal level. They determine how laws will be implemented or enforced by an agency and carry for the force of law.
What is the Palliative Care Policy GPS?
The GPS (pictured below) provides a regularly updated platform for surveying palliative care-relevant policies across the 50 states, Washington, D.C., the Indian Health Service, the Veterans Administration (VA), and the territories.
The GPS provides a regularly updated platform for surveying palliative care-relevant policies across the 50 states, Washington, D.C., the Indian Health Service, the Veterans Administration (VA), and the territories.
Data is displayed through a user interface that allows visitors to track bills and laws using several methods. Viewers can sort by location—whether by state, region, or other entity (such as the territories)—as well as by bill status, topic, and timeframe. Every piece of legislation is sorted by date, its status (e.g., whether a bill has been introduced, passed, or failed), and category. Each entry also provides a short content summary alongside a link to the legislation itself.
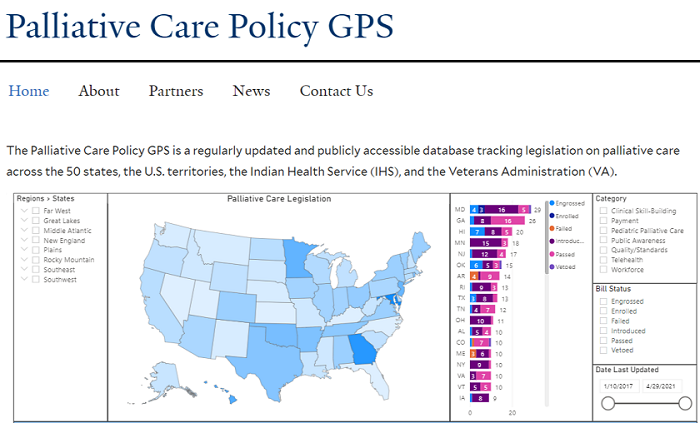
Legislation is tracked across seven categories:
1. Workforce
Laws and policies that support the growth of a specialty palliative care workforce (e.g., certification programs, loan forgiveness programs, etc.).
2. Payment
Laws and policies that expand financing or provide financing incentives to ensure access to palliative care (e.g., budget bills that appropriate funds for state-backed palliative care programs).
3. Quality/standards
Laws and policies geared toward developing and meeting quality metrics and standards for palliative care (e.g., safety standards).
4. Clinical skill-building:
Laws and policies that increase capacity of all health care professionals to (1) initiate meaningful communication with patients about what matters most to them, and (2) provide symptom relief, education, and other services to improve quality of life for people living with serious illness (e.g., clinician training in palliative care, continuing education in pain and symptom management, opioid prescribing, communication, family support, etc.).
5. Pediatric palliative care
Laws and policies that support the development and expansion of pediatric palliative care and pediatric hospice (as they relate to access, workforce, quality/standards, clinical skill-building, public awareness, etc.).
6. Public awareness
Laws, policies, and organizations that promote public awareness of palliative care (e.g., advisory councils, public health campaigns).
7. Telehealth
Laws and policies related to telehealth—of particular importance given the COVID-19 pandemic (ranging from state laws that define telemedicine and telehealth to legislation requiring coverage for telehealth services).
Presenting this information in one place will allow users to assess legislative developments over time, encouraging the identification of trends (both within and across categories), innovative policy initiatives, and best practices. Gaps in the policymaking space can be identified along the way, encouraging reform in the process. And through the identification of ideas and best practices implemented elsewhere, palliative care champions can work in concert with their own state policymakers to craft more effective laws bolstering palliative care. These advancements could ameliorate disparities in access to high-quality palliative care, expand the palliative care workforce, drive essential skills across key clinicians, and increase public awareness of palliative care.
Presenting this information in one place will allow users to assess legislative developments over time, encouraging the identification of trends, innovative policy initiatives, and best practices.
To better inform both research and advocacy, the GPS includes a wide range of legislation. It not only tracks bills that have successfully become laws, but also those that failed or evolved over time (appearing, for instance, as different bills in separate legislative chambers). This information will help users identify ideas that helped secure passage for meaningful legislation, while preserving proposals that did not quite make it across the finish line but that could nevertheless inspire future policy reform.
The GPS was designed with a broad audience in mind, ranging from health care professionals to policymakers, and is meant to empower all users during a transformative time for palliative care. While the GPS aims to expand beyond the states, territories, and IHS, it begins there because of the power of state-level policymaking—the database already contains hundreds of bills, indicating robust activity across states—along with a commitment to ensuring that IHS and the territories are included in the national policy dialogue. We aim to expand on this effort in coming months.
The GPS was designed with a broad audience in mind, ranging from health care professionals to policymakers, and is meant to empower all users during a transformative time for palliative care.
Future Work
While the GPS initially focuses on gathering legislation from across the 50 states, Washington, D.C., the territories, and the Indian Health Service, the second phase of this project will extend the tracker to cover regulations arising from each of these entities. State regulations play a number of vital roles, ranging from defining scope of services and patient eligibility to setting training requirements—including through Continuing Medical Education benchmarks. State regulatory entities can include: Departments of Health; Departments of Social Services; Departments of Insurance; and much more. This large number of relevant regulatory bodies makes maintaining an up-to-date database all the more important. Finally, in the project’s third phase, the GPS will extend to cover state regulations while adding monitoring of federal legislation. By including federal policy, the GPS will allow users to track how Congress and relevant agencies impact workforce (e.g., through training programs and grants), along with payment and quality (especially through the Center for Medicare and Medicaid Innovation models).
While expanding the scope of the GPS is a key priority moving forward, the database will also support innovative research as well as the development of tools to support effective advocacy. GPS data could help identify best practices for advancing meaningful palliative care policy—tracking innovative strategies as they emerge—while also spotlighting legislative trends across areas such as telemedicine and payment. The GPS site will also provide newcomers to the policy space with helpful information about the legislative process, describing key features of state lawmaking while also highlighting the rich diversity in state approaches to policymaking and palliative care. Primers on best practices and the legislative process could become useful tools for both experienced and emerging advocates. By weaving together the siloed landscape of state policymaking, the GPS offers an exciting new tool for the important work ahead.
To learn more about the Palliative Care Policy GPS, register for our upcoming webinar (August 12). Furthermore, if you have any suggestions for how to improve the GPS, or know of existing policies that could be included, please submit them here.
Additional Resources
For additional information relevant to the GPS, please refer to the following:
- Palliative Care Policy GPS
- Register for the GPS Webinar, 'How to Improve Palliative Care Access and Quality at the State Level' (August 12 at 12:30pm ET)
- CAPC's State Policy Resources Toolkit
- America’s Care of Serious Illness: 2019 State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals
- State Palliative Care Forum
- NASHP State Strategies to Build and Support Palliative Care
- CTAC State and Community Organizing Engagement Toolkit
Search the new online Palliative Care Policy GPS, which tracks individual state policies on palliative care.
Get Started
